While AI scribes are heralded as a breakthrough for reducing documentation burdens, experts caution that unanswered questions on reliability, ethics, and patient safety must be addressed before widescale adoption.
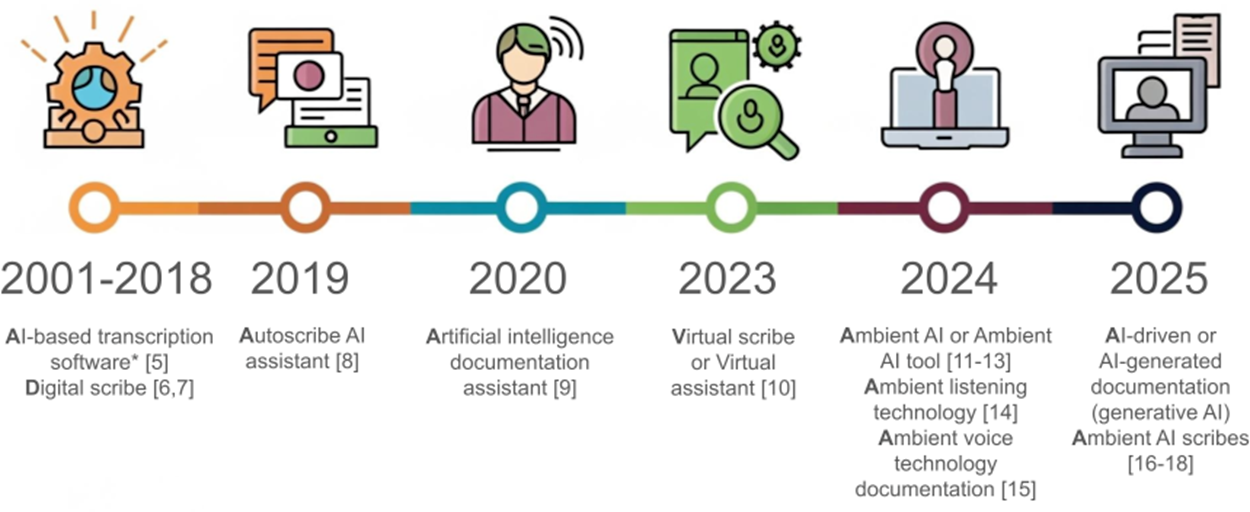
Terminology used for artificial intelligence (AI)–based documentation technologies, based on published literature over the past decade. Transcription software in this period was based on various types of AI models, including one or more of the following: automated speech recognition, natural language processing, probabilistic graphical models (such as conditional random fields), or logistic regression models.
A new editorial published in JMIR Medical Informatics examines the rapid rise of ambient artificial intelligence (AI) scribes, technologies designed to automate clinical documentation and alleviate the administrative burden on healthcare practitioners. While these tools show great promise in reducing burnout and freeing up time for patient care, the editorial highlights significant concerns that warrant further investigation. The editorial also serves as a formal call for papers, launching a new JMIR Medical Informatics section on ambient AI scribes and AI-driven documentation.
Potential Benefits in Clinical Practice
The piece, authored by Dr. Tiffany I. Leung, Dr. Andrew J. Coristine, and Dr. Arriel Benis, acknowledges the potential of ambient AI scribes to revolutionize clinical workflows. It notes that early evidence suggests these tools can lead to reduced clinician burnout, less time spent on after-hours documentation, and improved patient-physician interaction as providers can be more present during visits. Reported benefits are heterogeneous, varying by specialty and workflow, and most evaluations to date are small pilot studies.
Risks, Limitations, and Ethical Challenges
However, the authors caution that several challenges offset these benefits. The editorial points to persistent concerns about the accuracy and reliability of AI-generated notes, including errors, omissions, and hallucinations. It also raises ethical and legal questions, such as algorithmic bias, privacy risks, and the potential for "cognitive debt" or overreliance on AI, which could diminish critical thinking skills. Additional concerns include potential loss of physician autonomy, security and interoperability hurdles, user acceptance and training needs, and cost-effectiveness at scale. The authors also highlight the risks of note bloat and potential impacts on clinical reasoning and trainee learning. Evidence directly capturing the perspectives of patients and caregivers remains limited, highlighting a priority area for future research.
Call for Rigorous Research and Responsible Implementation
Although the enthusiasm for AI scribes is understandable, the medical community must proceed with caution and a commitment to rigorous, evidence-based evaluation. The analysis reveals that while these tools are a promising solution to a long-standing problem, numerous questions remain unanswered regarding their impact on patient safety, clinician training, and system-level outcomes. The editorial is non-peer-reviewed and discloses the authors’ editorial roles at JMIR, as well as the use of AI tools for summarization during manuscript preparation.
New JMIR Section and Call for Papers
This editorial highlights a critical need for more scholarly work to guide the responsible and effective deployment of AI scribes. To that end, JMIR Medical Informatics launched a new section and a call for papers on "Ambient AI Scribes and AI-Driven Documentation Technologies." The journal invites submissions of original research, implementation reports, and evidence-based perspectives from clinicians, patients, and health care leaders. Of particular interest are studies exploring the practical applications, challenges, and future directions of these technologies in real-world clinical settings.